Weight loss surgery Perth
Rachel had weight loss surgery and lost 23kg in 5 months.

Weight loss
surgery
If you have struggled to achieve or maintain weight loss long-term, you may be considering weight loss surgery, also known as bariatric surgery. We offer different types of obesity surgery, depending on your situation, for the management of obesity and related conditions such as diabetes.
Here, we answer your biggest questions about the surgery, including potential weight loss, dumping syndrome, and insurance coverage.
What is weight loss surgery?
How much weight can I lose with bariatric surgery?
So what surgery options are there?
Video: Types of weight loss surgery
What factors influence weight loss?
Surgical technique
Every surgeon does their operation slightly differently. For sure, a tighter sleeve will cause more weight loss. If too much stomach is left behind, (ie a loose sleeve), the results will not be as good.Genetics
If someone from your family has done well with surgery, you will do well also. The amount of weight loss is heavily dependant on how the operation influences the gut hormones, and this is genetically controlled.Medication
Many medications make you put on weight. (full list of medication that causes weight gain). Once we have done your surgery and you have recovered, it will be important to change any medications that make you put on weight to an alternative medication that does not cause (or has minimal) weight regain.
What you eat
Clearly if you stick to a healthy (lower calorie) diet you will do better than if you are eating calorie-dense foods like chocolate / junk food / alcohol / soft drinks. You are allowed to have these foods, but it’s all about moderating the quantity and frequency.
Have you had a prior gastric band?
Prior gastric bands limit the effectiveness of subsequent surgery, but we are not really sure why.
Theories why people with bands don’t do as well with subsequent surgery are:
- Bands cause oesophageal stretch, facilitating the oesophagus to behave like a second stomach thereby allowing clients to eat more.
- The possibility that the effectiveness of gut hormones is dampened by the prior band, and therefore the subsequent surgery doesn't have as much of a hormonal impact.
- The quality of the subsequent surgery is impacted by the scarring caused by the prior gastric band.
- That clients have learned to “cheat the surgery” and have developed bad habits. Clients with gastric bands often find softer, energy-dense foods are easier to consume and can fall into bad eating habits.
What is dumping syndrome in weight loss surgery?
This term is frequently overused. But true, dumping syndrome relates to what happens if sugar is allowed into the small intestine in large quantities. It happens in people that have had bypass operations, but may happen after sleeve gastrectomy as well. Dumping syndrome is said to occur in up to 50% of bypass patients and happens in stages.
Consuming a large amount of sugar that gets into the small bowel unchecked will result in the following:
Phase 1
The high concentration of sugar in the small intestine irritates the small bowel lining. The small bowel lining then starts to pour water into the small bowel to dilute the sugar. This means that water is moved out of the circulation into the bowel. This results in a fall in blood pressure, resulting in dizziness, palpitations, hypotension, sweating, headache, flushing, and disorientation. The feeling of needing to sit down. This often happens 15-30 minutes after eating a sugary meal.Phase 2
The sugar gets absorbed, pushing the blood sugar very high.Phase 3
In response to the high blood sugar there is a surge in insulin release, causing the blood sugar to fall to a very low level. This will cause headaches and fainting.Phase 4
Late dumping occurs 2-3 hours after the meal. Unabsorbed sugar reaches the colon where bacteria ferment it, causing gassy diarrhoea.How is dumping syndrome best treated?
- Firstly, control diet, in particular by avoiding sugary foods in your diet.
- Secondly, we have medications that can help.
- Finally, it may be possible to undo the surgery and thereby, reduce the dumping.
How does weight loss surgery reverse diabetes?
The effect of weight loss surgery on diabetes is almost magical. Often clients find that their diabetes has gone into remission and they no longer require any medication.
We never say cured as diabetes seems to sit in the background. It may come back at a later time, but it can be in remission for as long as 10-20 years, and this is a major advantage to your long term health.
The way this happens is not known, but theories are:
- The hormonal effect of the surgery has a major influence on insulin production and insulin sensitivity.
- Reducing weight reduces insulin resistance, and this makes the available insulin work more effectively.
- Eating less means a lower carbohydrate load with meals, so the sugar load is not as great.
Weight loss surgery is most effective if done quickly after a diagnosis. If the diagnosis of diabetes was made less than two years prior to surgery, there is an 80% chance of getting off all diabetes medication. Often, if diabetes is improved and medication can be reduced, the progression to needing insulin less likely. But the effectiveness of the surgery diminishes in people who have had diabetes for longer periods of time.
We (and the Australian Diabetes Foundation) recommend having weight loss surgery as soon as possible after a diagnosis of diabetes is made.
Bypasses are slightly more effective in controlling diabetes, but they also have their drawbacks.
Can I get a second opinion?
Absolutely. We are very keen that you do so and we are happy to point you in the right direction. We belong to a group of bariatric surgeons in Perth that are both experienced and capable. A second opinion is always valuable, either to hear the same ideas from a different perspective or to get fresh eyes on a problem, and maybe some extra ideas. If you would like a second opinion just ask.
We are also happy to provide a second opinion on an existing problem. You’ll find that we have a few tricks up our sleeve.
Is obesity a disease or a risk factor?
This is the source of much debate amongst doctors, and a conclusive decision has not been reached yet. I feel that obesity is a syndrome, made up of different diseases and disease processes, that make you put on weight.
Figuring out what makes an individual person put on weight is hard, but important, as this is where the therapy needs to be targeted. Surgery will lower your weight, but it’s endpoint effectiveness relies on managing the other issues as well.
So what’s the big deal?
The terrible social stigma of being overweight and all the issues that that carries I believe are more important than what I’m about to tell you. Medically speaking, obesity is a risk factor for many diseases, and unfortunately, it will shorten your life expectancy. It’s when you look at the numbers that the truth becomes undeniable.
With a BMI of 40 or over your chance of reaching the age of 60 is 76%. That is a one in three chance of dying by the age of 60. This is why the government permits you to access the early release of money from your superannuation fund to cover the cost of your entire (or even only part of your) medical expenses related to your obesity surgery.
This is available to both privately insured and uninsured clients but is governed by some very strict guidelines (see below).
How do I access my superannuation to fund my surgery
Life-threatening conditions (causing death within twelve months)
Psychiatric conditions
Management of chronic pain - we prefer to use this option. Most people needing bariatric surgery have pain, Usually in their back, sometimes knees and hips and lots of other places. By losing weight and taking the load off these joints pain improves and this qualifies us to use this clause.
The administration of the early release of superannuation is performed by the Australian Taxation Office. They require a form to be completed, a letter from your GP and a letter from your surgeon. We recommend using a company called Supercare to help you process the paperwork. They are very helpful as they have a very good understanding of all the details necessary to make the process as smooth as possible. If you would rather attempt this yourselves our staff will be happy to guide you through the details as much as possible, but due to ATO privacy laws, we are unable to do the application for you.
FAQ
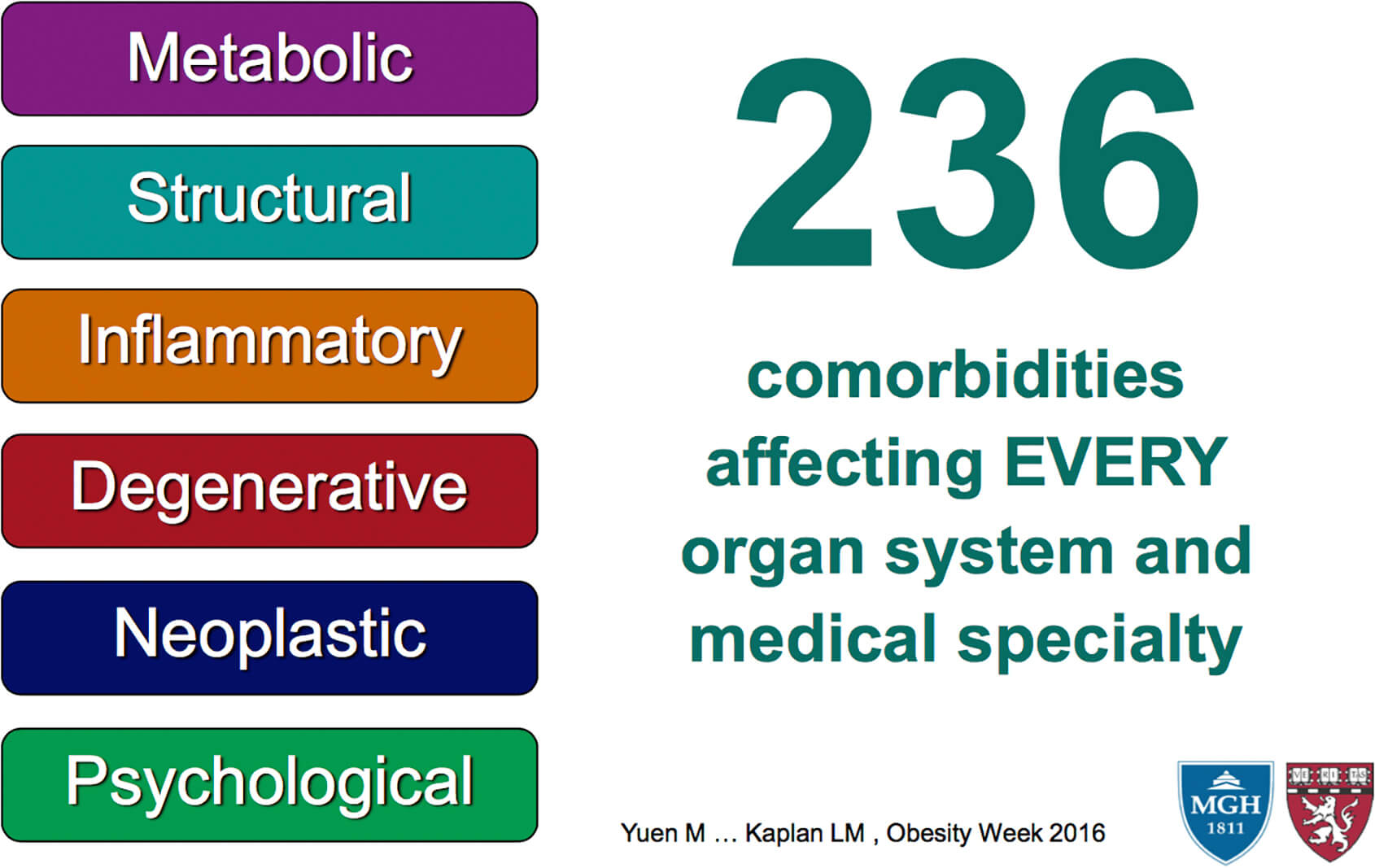
Medical complications of obesity
About Obesity Surgery WA: Our 6 commitments
Taking surgery seriously
We know that entering into an operation is a big deal and we are very serious in getting the best outcome for you. We practice what is considered to be a world class standard. Our staff regularly attend national and international conferences and bring back what is the latest research and technology.Running on time
Our Surgeons and all of our staff try their best to run on time. Although it's not always possible, our commitment is that we do our best. Your time is valuable and we respect that.Readily available
Our surgeons (or at least one of them) are always available in a crisis. Some of them may provide you with a direct contact, but all are available through the hospital switchboard and happy to chat any time if there is a crisis.An obsessive attention to detail
We do our best to not miss anything. Every stitch, every staple and every clip is applied to exactly where it needs to be with the greatest care possible.Commitment to performing the best operation possible
Not all operations are the same and there a few extras that we do to make things better. We know that our results are better with the minimiser ring so we offer it to everyone. We know that reflux can be an issue so we try to tighten every oesophageal hiatus to make reflux control as good as possibly can be.A commitment to new technologies
- We have brought in STRETTA into Western Australia, which we believe will revolutionise reflux management. (Have a look at the Stretta page for more information).
- SJOG Murdoch has just purchased a new DaVinci robot and we believe that this will allow us to do operations with keyhole surgery that previously needed a major laparotomy incision. Lynx is on the horizon and promises to also help manage reflux, we hope to have access to this in early 2020.
Useful links
Gastric
sleeve
Gastric
bypass
Roux-en-Y
Meet our team

Dr. Harsha Chandraratna
Consultant Surgeon
MBBS FRACS

Dr. Bill Gong
General and Laparoscopic Surgeon
MBBS FRACS

